Pay Online
Grasping Periodontal Disease and Its Effects
The term "periodontal" refers to the area "around the tooth." Periodontal disease, also known as periodontitis or gum disease, is a common inflammatory condition that affects the supporting tissues of the tooth, including the gums and jawbone, especially in its advanced stages.
Periodontal disease often begins with gingivitis, a bacterial infection of the gum tissue. When plaque toxins irritate and inflame the gums, a bacterial infection can develop. If this infection spreads to the gum pockets between the teeth, it becomes harder to treat and remove. As periodontal disease progresses, it destroys connective tissue and jawbone. If left untreated, it can cause tooth shifting, looseness, and eventually, tooth loss.
Periodontal disease is the leading cause of tooth loss in adults in developed countries and should be treated promptly to prevent further complications.
Types of Periodontal Disease
When left untreated, gingivitis (mild gum inflammation) can progress below the gum line. As plaque toxins irritate the gums, a chronic inflammatory response triggers the body to break down its own bone and soft tissue. Periodontal disease may have few or no noticeable symptoms, but it causes the teeth to separate from the infected gum tissue. Deepening pockets between the gums and teeth often indicate that both soft tissue and bone are being damaged by the disease.
Here are some of the most common types of periodontal disease:
- Chronic Periodontitis – Inflammation of the supporting tissues causes deep pockets and gum recession. While it may appear that the teeth are lengthening, the gums (gingiva) are actually receding. This is the most common form of periodontal disease and is characterized by progressive loss of attachment, with periods of rapid progression.
- Aggressive Periodontitis – This type of gum disease occurs in an otherwise healthy individual. It is marked by rapid loss of gum attachment, ongoing bone destruction, and often runs in families.
- Necrotizing Periodontitis – This severe form of periodontal disease typically affects individuals with systemic conditions such as HIV, immunosuppression, or malnutrition. It leads to necrosis (tissue death) in the periodontal ligament, alveolar bone, and gingival tissues.
- Periodontitis Caused by Systemic Disease – This type of gum disease often develops at an early age and is commonly associated with medical conditions such as respiratory disease, diabetes, and heart disease, which act as contributing factors.
Treatment for Periodontal Disease
Depending on the condition of your teeth, gums, and jawbone, your periodontist may recommend either surgical or nonsurgical treatments. Before any treatment is performed or recommended, a thorough periodontal exam of your mouth will be conducted.
Here are some of the most common treatments for periodontal disease:
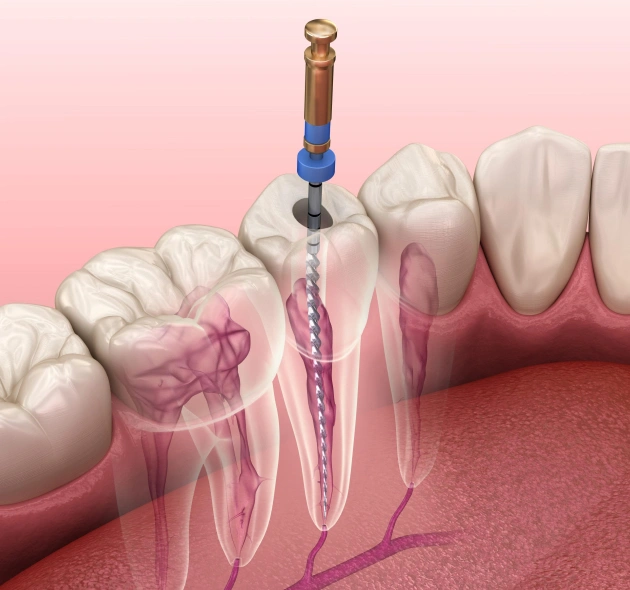
- Scaling and Root Planing – To protect gum health, bacteria and calculus (tartar) that caused the infection must be removed. The gum pockets will be cleaned and treated with antibiotics, if necessary, to help combat the infection. A prescription mouthwash may also be recommended as part of your daily oral care routine.
- Tissue Regeneration – When bone and gum tissue are lost, regrowth can be stimulated through grafting procedures. A membrane may be placed in the affected areas to support the regeneration process.
- Pocket Elimination Surgery – Also known as flap surgery, this surgical procedure is used to reduce the pocket size between the teeth and gums. Surgery on the jawbone may also be performed to smooth out indentations that encourage bacterial growth.
- Dental Implants – For teeth lost due to periodontal disease, dental implants can restore both the function and aesthetics of your smile by placing prosthetic teeth into the jawbone. Tissue regeneration procedures may be needed beforehand to strengthen the bone and support successful implant placement.
